Are you unsure about what’s right for your digestive health? You’re not alone!
Peptic ulcers are common, and myths about their symptoms, management, diet, and lifestyle can make it hard to know what’s true and how to take care of your gut effectively.
Let’s clear up these myths and understand the reality so you can manage your gut health with confidence
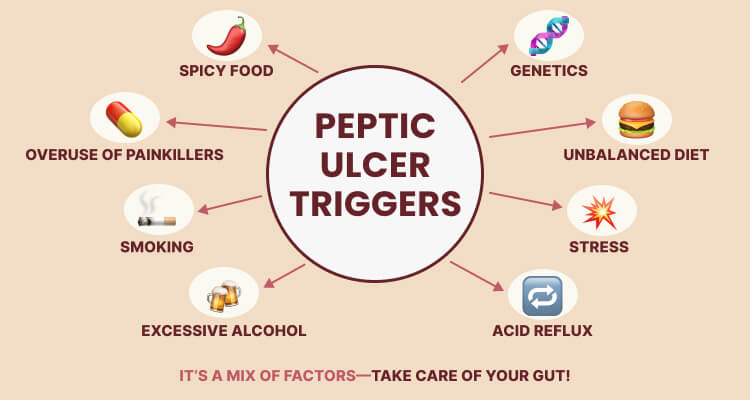
Myth 1: Eating spicy food is the sole reason for peptic ulcers.
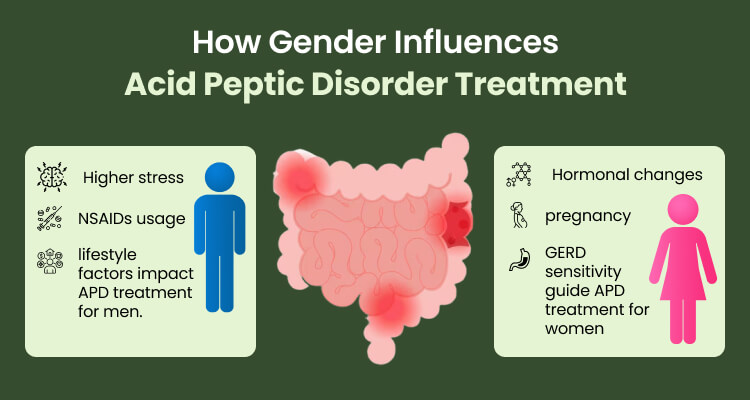
Many people see spicy foods as the enemy of the stomach. While it’s true that spicy dishes can irritate an already sensitive stomach, they may not be the direct cause of ulcers. The real culprits could be H. pylori infections and long-term use of NSAIDs like ibuprofen.
Research indicates that H. pylori is present in approximately 70-90% of individuals who experience peptic ulcers. Therefore, you should get tested for H. pylori.g.
Myth 2: Dairy milk is a long-term solution to heal peptic ulcers.
A common belief is that sipping a glass of dairy milk will soothe peptic ulcer discomfort. While it may provide temporary relief by coating your stomach, it can trigger stomach acid production, resulting in greater discomfort later on.
The misconception comes from the initial soothing effect, but milk can worsen symptoms. Instead, for acid peptic reflux, you can try these herbal teas to soothe symptoms:
- Chamomile Tea: Reduces inflammation and soothes the stomach lining
- Licorice Root Tea: Helps coat and protect the esophagus and stomach
- Fennel Tea: Helps digestion and reduces bloating without increasing acid production.
What to Avoid
-
- Peppermint Tea – Can relax the esophageal sphincter and worsen reflux.
- Ginger Tea (in excess) – While helpful for digestion, too much can increase acid production.
Myth 3: I’m too young to worry about acid peptic ulcers.
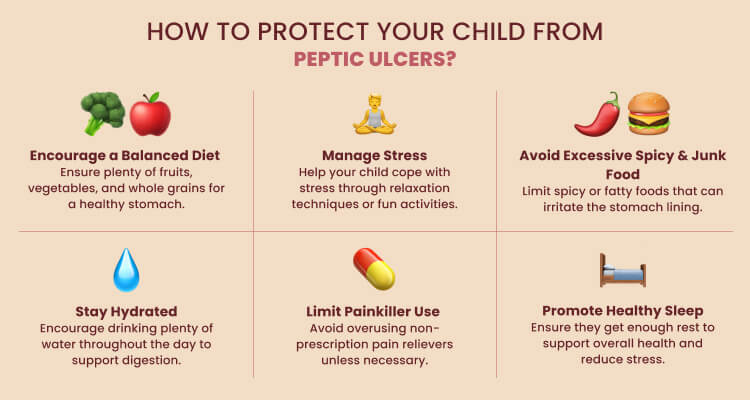
It’s easy to fall into the trap of thinking that acid peptic disease is an issue for older adults only. However, the truth is that this condition can affect people of all ages, including children and young adults.
Factors like diet, lifestyle, genetics, and H. pylori infections increase risk, making awareness important for everyone. Holistic care goes beyond symptom relief, focusing on a balanced diet, lifestyle, and emotional health. Paying attention to early symptoms and seeking timely guidance can prevent complications and support lasting wellness.
Myth 4: I’ll have to take medication for life if I have acid peptic ulcers.
Many people believe that once diagnosed with acid peptic ulcers, they will need to rely on medication permanently. However, this is not necessarily true. While medications such as proton pump inhibitors (PPIs) or H2 blockers may be prescribed for short-term relief and healing, long-term management can often be achieved through dietary and lifestyle changes.
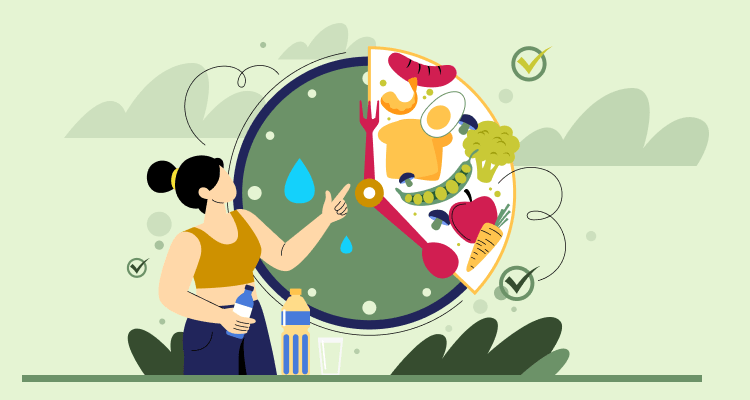
A gut-friendly diet plays a crucial role in ulcer healing and prevention. Eating more fiber-rich foods, fruits, vegetables, nuts, and seeds promotes digestive health, while cutting down on sugar, fried foods, alcohol, caffeine, and acidic items prevents irritation.
Managing stress, eating mindfully, and treating H. pylori infection from the root cause can reduce the chance of ulcers coming back and lower the need for long-term medicines.

Myth 5: Antacids alone can cure peptic ulcers.
You might say, “I just take antacids whenever I feel discomfort.”
However, while antacids can provide temporary relief from ulcer symptoms by neutralizing stomach acid, they do not address the underlying causes of peptic ulcers.
Simply taking antacids does not eliminate H. pylori bacteria or heal the stomach lining from NSAID-induced damage. A proper treatment plan may include antibiotics (for H. pylori), proton pump inhibitors (PPIs), or H2 blockers, along with dietary and lifestyle changes. Supporting healing with gut-friendly foods, supplements like probiotics and licorice, stress-reducing practices such as yoga and meditation, and mindful eating can improve recovery and prevent recurrence.

Myth 6: I believe stomach peptic ulcers are not a serious health condition.
Some might underestimate their stomach issues, thinking, “It’s just a little discomfort; how serious can it be?”
However, downplaying digestive issues can be risky. While mild cases may cause discomfort, persistent ulcers can result in internal bleeding, perforation (a hole in the stomach or intestine), and even life-threatening infections like peritonitis. Additionally, long-term ulcers increase the risk of stomach obstruction, making it difficult for food to pass through the digestive tract.
If you suspect you have a peptic ulcer, it’s essential to seek medical advice early. Prompt treatment can prevent complications and ensure long-term digestive health.
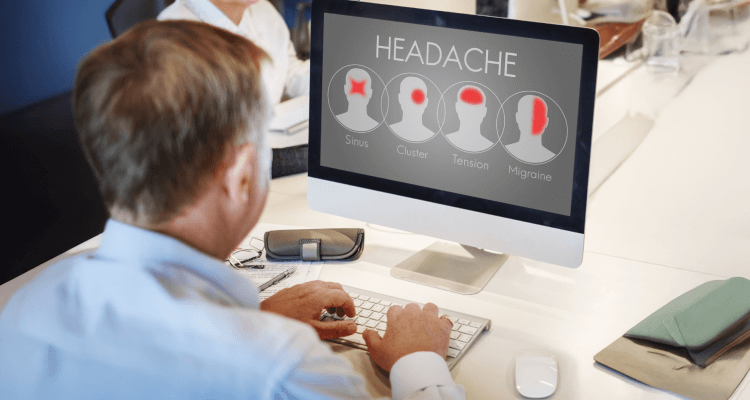
Myth 7: I don’t have any symptoms like heartburn, so I can’t have acid-peptic disease.
It’s easy to think that if you don’t have classic symptoms like heartburn, you’re in the clear. But acid-peptic disease (APD) isn’t always obvious. Some people go for months or even years without realizing they have it, because the symptoms can be silent or unusual.
Instead of heartburn, you might feel bloating, nausea, fatigue, or even a loss of appetite. Some people only find out they have an ulcer when it starts bleeding, leading to anemia or black, tarry stools. Others don’t notice anything until they develop serious complications like a perforated ulcer (which is as painful as it sounds).
Just because you’re not feeling the burn doesn’t mean your stomach isn’t struggling. Pay attention to small signs, like frequent indigestion, unexplained discomfort, or changes in appetite.
Even if you feel fine, taking care of your gut (by eating more fiber, cutting back on alcohol and fried foods, and managing stress) can go a long way in preventing problems before they start.
If something feels off, don’t ignore it. Your stomach will thank you later.
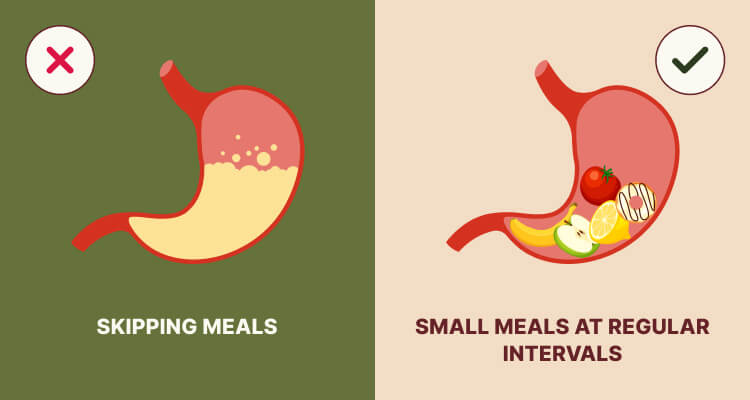
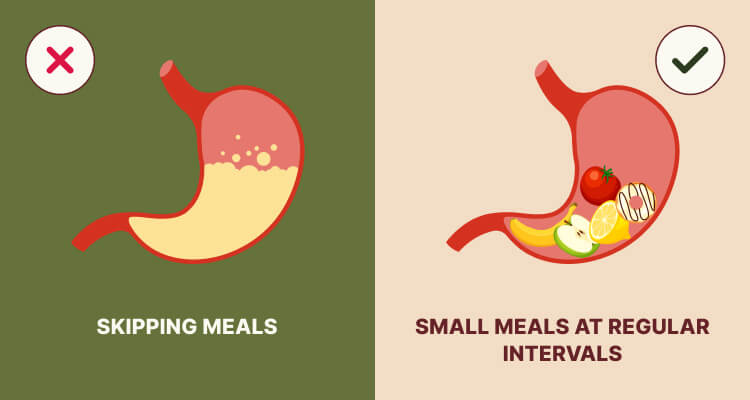
Myth 8: I can reduce peptic ulcer symptoms by eating less.
It may seem smart to eat less with an ulcer, but skipping meals can make symptoms worse. An empty stomach allows acid to build up, which irritates the ulcer and causes more pain, bloating, and discomfort.
Rather than eating less, try having small, frequent meals that include fiber, lean proteins, and probiotics (such as oats, bananas, yogurt, and vegetables). These foods help soothe the stomach and aid healing. Skipping meals or going too long without food can increase acid and worsen symptoms.
If you have a peptic ulcer, it’s not just about how much you eat. It’s also about what and when you eat. Listening to your body and eating mindfully can help keep symptoms in check and promote healing.
Myth 9: I’ll always have chronic acid peptic ulcers.
Some may worry that being diagnosed means they’ll have to deal with ulcers for the rest of their lives. However, that’s not the case for everyone. The truth is, most ulcers can be healed with the right approach.
In addition to medical treatments, Live Your Best Life offers a holistic approach to help manage and prevent ulcers. It focuses on balancing the body’s energies (doshas) to promote healing. For ulcers, this often means focusing on cooling foods and herbs that soothe the stomach, like aloe vera and licorice root. It also suggests avoiding spicy and acidic foods and managing stress through practices such as yoga and meditation.
Whether you prefer modern medicine or natural remedies, the key is that ulcers can heal with the right approach, and you don’t have to live with them forever.

How Can You Embrace Holistic Healing for Peptic Ulcers with the Live Your Best Life Approach?
When it comes to treating ulcers, Ayurveda takes a personalized approach, focusing on your unique body constitution and the specific manifestation of your condition. There are three main principles at play here:
-
Balancing Doshas
Here, the focus is on calming your Pitta dosha, which is often aggravated in cases of peptic ulcers.
Ayurvedic practitioners may recommend natural remedies and herbs known for their soothing properties. Licorice is recognized for its ability to coat and protect the stomach lining, while raisins or grapes can aid digestion and provide nourishment, making them beneficial for those experiencing ulcers.
In some cases, an Ayurvedic expert may recommend Panchakarma, a deep detoxification that uses therapies such as purgation or medicated enema to restore balance and support digestive health.
-
Avoiding Aggravating Factors
Managing peptic ulcers means avoiding foods that irritate your stomach. Common triggers include spicy dishes, caffeine, and alcohol, as they increase acidity and discomfort. Instead, we encourage you to eat gentle, nourishing foods, such as fruits, vegetables, and whole grains that support healing and keep your digestion comfortable.
-
Lifestyle Changes
Along with diet, holistic healing also depends on your lifestyle. Practices such as yoga, meditation, and deep breathing help reduce stress, which often worsens digestive problems. Gentle, regular physical activity that feels comfortable for your body will further support both your digestion and overall well-being.
Are You Ready to Nurture Your Digestive Health?
Peptic ulcers are often misunderstood, surrounded by myths that create fear, confusion, and sometimes even delays in proper care. Clearing these misconceptions is the first step toward proper management. At Live Your Best Life, we help you move beyond myths by combining Ayurvedic wisdom with modern insights, so you not only understand the true causes of ulcers but also discover safe, holistic, and effective ways to heal your gut.
Our integrated approach combines Ayurvedic wisdom with practical lifestyle changes and evidence-based herbal supplements to restore lasting balance.
We design personalized care plans that include soothing herbal formulations to protect the stomach lining, tailored diet guidance to reduce irritation, and simple lifestyle practices such as mindful eating, yoga, and stress management. We also integrate modern insights for monitoring progress.
By addressing both immediate discomfort and long-term digestive resilience, we empower you with holistic, sustainable solutions—helping you move beyond myths and quick fixes to achieve lasting relief, renewed energy, and a healthier gut.